I’ve been pushing the cannabinoid system because no one talks about it. For many of the people who read my blog, it’s the single most important pathway.
The Thin Anxious Person: An Underactive Cannabinoid System
Someone with an underactive cannabinoid system will not get the same rewarding aspects of food and sex. Such people might not value these things as much, and it may manifest as a lower libido.
They are predisposed to an autoimmune condition, especially one involving the gut, because the cannabinoid system is very protective against autoimmune inflammation.
The cannabinoid system is very highly concentrated in the hypothalamus, basal ganglia, and the hippocampus, which are part of the limbic system.
People who have an underactive cannabinoid system will get more anxiety and limbic system problems in response to inflammation.
They might have some GI disturbances because of increased anxiety and lowered cannabinoid function.
These people will not get hungry very often and more likely eat to get energy. When they do eat, they will be more likely to burn it and not as fat. This is from a dysfunctional cannabinoid system. Blocking the CB1 receptors increases insulin sensitivity and the burning of fatty acids in muscles and the liver [1].
They will be more anxious and more likely to have food sensitivities because the cannabinoid system is very important for emotional balance and creating tolerance to our environment, especially food that interact with our gut.
Such people tend to have higher adiponectin, higher growth hormone (cannabinoids inhibit growth hormone release [2]), lower triglycerides, higher HDL, lower insulin resistance, lower CRP and higher TSH, but not higher T4/T3 [cannabinoids decrease TSH 3].
Having lower cannabinoid function is consistent with these symptoms.

Brain Fog Meets Cannabinoids
The lateral hypothalamus is home to the neuropeptide orexin.
The lateral hypothalamus (mainly via Orexin) promotes brain function, motivation, hunger, wakefulness, energy expenditure/warmth [4], intestinal flow and gastrointestinal function by way of the dorsal nucleus of the vagus nerve and reduces pain [5].
It increases motivation through the ventral tegmental area (VTA) and other areas of the reward system [5].
It regulates neuroendocrine functions (e.g., HPA axis, HPG axis, and HPT axis) through other parts of the hypothalamus. This neuroendocrine role impact most of the significant hormones in your body, including stress hormones, sex hormones, and thyroid hormones.
The lateral hypothalamus regulates respiration, blood pressure, and urination via a group of structures in the brain stem, among other functions
My clients with limbic system issues (almost all of them) display:
- Brain fog
- Fatigue
- Insomnia
- Lower motivation
- Depressed appetite
- Cold hands and feet
- Gut problems including constipation
- Sometimes pain
- Lower thyroid and sex hormones
- Overstimulated HPA axis
- Lower blood pressure
- Frequent urination
If you compare these symptoms to the functions of the lateral hypothalamus, you will notice it’s pretty similar. The lateral hypothalamus doesn’t accomplish all of these tasks independently, but more like gives commands to other parts of the limbic system.
The lateral hypothalamus coordinates with and gives messages to the rest of the hypothalamus. The hypothalamus is the processor of the brain and the key part of the limbic system.
Our cannabinoid system and orexin system are closely intertwined, and they have a significant overlap in their function and location [6].
The CB1 receptor and Orexin 1 receptor combine and produce a 100-fold amplification of the potency of the orexin receptor 1-mediated function (via ERK) [6].
CB1 and CB2 receptors are most highly concentrated in the limbic system, the same brain network that mediates all of the symptoms displayed by my clients.
This is not a coincidence.
Conclusion: Adrenal fatigue is a misunderstanding of biology. It’s simply limbic system dysregulation, and altered cannabinoid function within the limbic system is at the core of causing these issues.
See tips on how to strengthen cannabinoid system without pot.
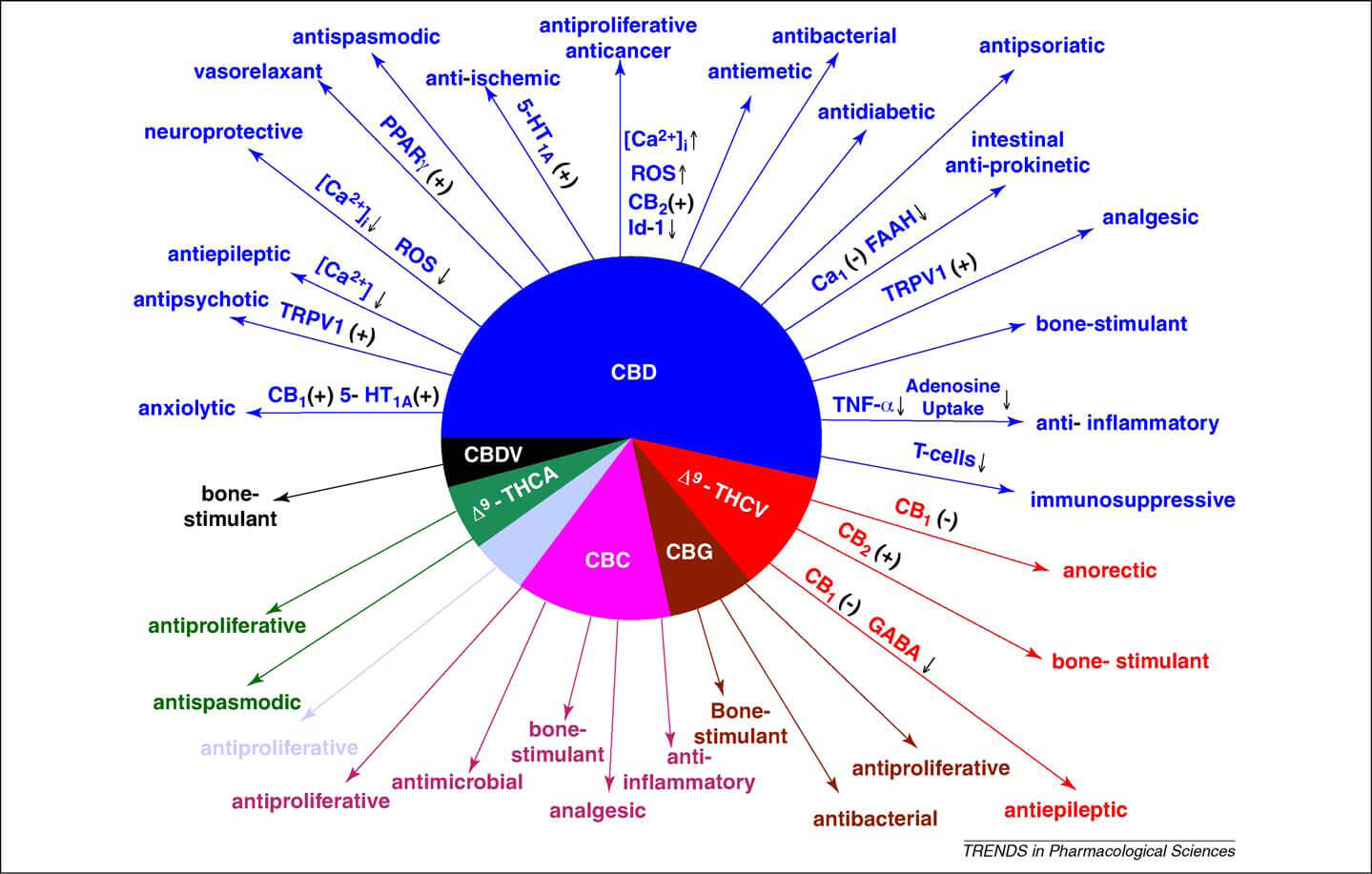
The Cannabinoid CB1 vs CB2 Receptor
CB1 receptors are found primarily in the brain, more specifically in the basal ganglia and in the limbic system, including the hippocampus [7, 8].
CB2 receptors are predominantly found in the immune system, with the greatest density in the spleen. CB2 receptors appear to be responsible for the anti-inflammatory and possibly other therapeutic effects of cannabis seen in animal models [9].
The 2 Main Natural Cannabinoids Found in the Body
Anandamide or AEA
The name is derived from the Sanskrit word for ananda, which means bliss and -amide. It has a pharmacology similar to THC, although its structure is quite different. Anandamide binds to the CB1 and, to a lesser extent, CB2 cannabinoid receptors.
Anandamide is about as potent as THC at the CB1 receptor. Anandamide is found in nearly all tissues in a wide range of animals. Anandamide has also been found in plants, including small amounts in chocolate.
Other similar natural molecules include PEA (palmitoylethanolamide) and OEA (oleoylethanolamide), which possess anti-inflammatory and hunger promoting effects, respectively. PEA cannot strictly be considered a classic endocannabinoid because it lacks affinity for the cannabinoid receptors CB1 and CB2. However, the presence of PEA has been known to enhance anandamide activity.
2-Arachidonoylglycerol or 2-AG
2-AG binds to both the CB1 and CB2 receptors with similar affinity, acting as a full agonist at both.
2-AG is present at significantly higher concentrations in the brain than anandamide, and there is some controversy over whether 2-AG rather than anandamide is chiefly responsible for cannabinoid function in organisms.
CB1 Receptor: The Good
The cannabinoid system plays an important role in neural plasticity, stress response, and learning and memory [10].
1) CB1 Lowers Anxiety and Stress
Mice without CB1 receptors appear more anxious (less GABA and higher glutamate function) and have an enlarged amygdala. Overall, strong converging genetic studies indicate that CB1 receptors are important for reducing anxiety, particularly during times of high-stress periods [11].
CB1 receptors are found in particularly high density in the hippocampus and amygdala, regions are known to play a role in emotional regulation and memory, and regions suggested to play a role in ADHD, emotional regulation, and other psychiatric disorders (e.g., bipolar, mood, anxiety disorders) [10].
CB1 receptors are found primarily in the brain and appear to impact predominately the GABA and Glutamate systems [11], but also affects the dopamine and serotonin systems.
As far as brain regions, the anti-anxiety effects of Cannabinoids seem to be from its effects on activating prefrontal cortex (PFC) and shutting down the amygdala, two structures commonly involved in anxiety. Anxiety is typically associated with reduced activity in the Prefrontal and enhanced activity in the amygdala [11].
Individuals who did not mount a 2-AG (internal cannabinoid and CB1 activator) response to stress exposure exhibited dramatically higher levels of cortisol [11].
Drugs that block the cannabinoid receptor
There was approximately a threefold increase in anxiety symptoms compared to the placebo with one anti-cannabinoid drug, and these studies were all performed on individuals who had no history of psychiatric illness [11].
One case report discusses a severe bout of depression, which subsided following cessation of the drug [11].
The CB1 blocking drug made people more negative and pessimistic activated the HPA axis and blunted pleasure to things (anhedonia) [11].
2) CB1 Alleviates Post Traumatic Stress Disorder (PTSD)
There is strong evidence that the cannabinoid system as a whole is required for appropriate adaptation and buffering of stress in humans [11].
Psychological stress decreases anandamide (internal cannabinoid) levels in multiple limbic brain regions (involved with emotion, cognition), but more robustly in the amygdala – and the reduction lasts at least 24 hours [11].
It’s believed that the reduced anandamide is responsible for at least some of the cortisol release from psychological stress [11].
Acute disruption of CB1 receptor reliably increases anxiety, impairs our ability to handle stress and activates the HPA axis [11].
Cannabinoids in the prefrontal cortex can enhance neuronal activity through a suppression of GABA release while suppressing glutamate release and excitability within the amygdala (dendrites) [11].
Clinical studies with CB1 receptor activators have shown therapeutic benefit in the treatment of both generalized anxiety conditions and post-traumatic stress disorder (PTSD) [11].
In humans, regular cannabis use can effectively dampen activation of the amygdala in response to stressful conditions [11].
A recent report found anandamide and 2-AG are significantly lower in individuals with PTSD, compared to both healthy controls and those exposed to trauma who did not develop PTSD [11].
Chronic stress in mice without CB1 receptors show an enlarged fear center or amygdala (dendrites) [11].
3) CB1 Ameliorates Depression
It has also been found that individuals who had post-surgical depression also had low levels of Anandamide and 2-AG [11].
The lower anandamide levels in people, the higher the anxiety scores, both in a healthy population and in those with major depression [11].
Women with lower 2-AG had higher rates of depression [11].
People with more anandamide (internal cannabinoid and CB1 activator) after a stressful event had less cortisol [11].
Interestingly, people with higher Anandamide and 2-AG were found to be at higher risk for minor depression. Researchers believe that these CB1 activators may curb the development of major depression [11].
4) CB1 Helps Induce Sleep
In rats, cannabinoids increase slow wave sleep and rapid eye movement sleep [10].
5) CB1 Increases Myelin and BDNF
The CB1 cannabinoid receptor can increase myelin formation in cells [12].
Mice without CB1 receptors have reduced hippocampal (memory center) BDNF [11].
Chronic CB1 blocking causes depression and actually decreases neurotransmitter and BDNF levels.
6) CB1 Lowers Intestinal Inflammation
Studies indicate that the gut nervous system is the main site of CB1 receptors [13].
The cannabinoid system is also important in dampening intestinal inflammation in humans [14].
Cannabinoid activation decreases intestinal permeability [15].
7) CB1 and CB2 Suppress Mast Cells
Mast cells contain CB1 and CB2 receptors, which when activated inhibit mast cell release [16].
8) CB1 Lowers Blood Pressure
Activation of the CB1 receptor can lower blood pressure [17].
CB1 Receptor: The Bad
1) Cognitive function
Cannabinoids impair memory and increase fatigue [10].
Activation of the CB1 receptor can lower cognitive performance by decreasing acetylcholine, glutamate, long-term potentiation and cyclic AMP [18].
THC produced dose-dependent impairments in immediate and delayed recall of a word list in healthy subjects [19].
THC impairs immediate and delayed recall of a word list, verbal learning and recall, sustained attention, selective attention, and motor speed in healthy subjects. Cannabinoids impair learning, short-term memory, working memory, executive function, abstract ability and decision-making in humans [19].
2) Anxiety
Unexpectedly, in some cases (such as alcohol withdrawal), activation of the CB1 receptor can contribute to anxiety [11].
3) Bone Density
CB1 receptor activation decreases bone density [20].
4) Constipation
Activation of the cannabinoid receptors can inhibit intestinal flow [21, 22, 23].
5) Liver fat
Activation of CB1 in mice increases liver fat (via SREBP-1c) [24].
6) Weight Gain

In humans, blocking the CB1 receptor helps people lose weight and also alleviates metabolic abnormalities associated with obesity; however, drugs tested for this were removed because people developed anxiety and depression [11].
Animal data indicate that CB1 activation has other weight gaining mechanisms besides increased food intake.
Activation of CB1 results in increased food intake [25], insulin resistance [26, 27, 28, 29], liver fat [30, 31, 32], and reduced fatty acid β-oxidation [33, 34].
CB1 activation prevents the breakdown and burning of fat cells for energy. In white fat, the activation of CB1 inhibits the secretion of adiponectin, and in brown fat CB1 activation decreases the thermogenic factor, UCP-1 [35].
Chronic CB1 blockade or genetic knockout of CB1 results in decreased food intake, body weight, and fat, increased insulin and leptin sensitivity, and improvements in glucose and lipid homeostasis in rodent models of obesity and similar effects were reported in obese subjects treated with a drug that blocks the CB1 receptor [36].
7) Cancer
The CB1 receptor may participate in brain cancer, as there are more receptors in tumors [37].
8) Psychosis
There are a number of anecdotal reports that cannabis can produce a range of acute psychotic symptoms that include depersonalization, derealization, paranoia, ideas of reference, flight of ideas, pressured thought, disorganized thinking, persecutory delusions, grandiose delusions, auditory and visual hallucinations, and impairments in attention and memory in an otherwise clear consciousness [19].
In recent years, there has been research linking cannabis use and schizophrenia-like psychotic disorders, and epidemiological evidence consistently suggests that the use of cannabis during adolescence increases the risk for psychotic disorders by 2-fold.
Read more about cannabis-induced psychosis.
Circadian Rhythm and CB1 Receptor
Cannabinoids tend to generate a distorted sense of time [38].
The CB1 receptors are abundant on the master circadian timekeeper (SCN) [38].
Cannabinoids lessened the ability of the circadian clock to entrain to light (phase advance) [38].
Mice without CB1 receptors have disrupted circadian rhythms and increased CRH/HPA activation, especially in their subjective mornings, and less cortisol sensitivity in their hypothalamus [39].
CRY1 gene expression is associated with the CB1 receptor expression [40]. CRY1 is increased by SIRT1.
CB1, Hormones, and Pathways
Activation of the CB1 or CB2 receptor inhibits cyclic AMP [18]. This is one of the ways by which cannabis can hurt cognitive function. When I was doing experiments with cannabis, some of the negative effects on cognitive function were reversed by forskolin.
Activation of the CB1 receptor lowers adiponectin [36]. Adiponectin is higher in people with lectin sensitivity, and adipinectin can cause inflammation in some ways.
At socially relevant doses, THC raised cortisol levels in a dose-dependent manner but frequent users showed blunted increases relative to healthy controls [41].
THC and cannabinoid activation (CB1) decrease prolactin [42]. Frequent users also had lower baseline plasma prolactin levels relative to healthy controls [41]. Prolactin is on the whole an inflammatory hormone and this can help lower inflammation.
Cannabinoids are also known to increase CCK [10] and ghrelin release [43].
CB1 receptor activation decreases thyroid hormones (especially TSH) [3] and I’ve found a synergy between cannabis and increasing thyroid hormones.
Regarding growth hormone, THC increased growth hormone, while anandamide decreased it [3].
Activation of the CB1 receptor inhibits both glutamate and GABA [44].
CB1 receptor activation increases PPAR gamma [45].
Endocannabinoid are natural PPAR Alpha activators [46, 47].
CB1 Receptor SNPs/Genes (CNR1)
Main SNP: RS1049353 (CNR1)
I call this SNP the lectin sensitive gene because this SNP has a big influence on how likely someone will have symptoms of limbic system problem from food sensitivities.
Each T of the SNP rs1049353 contributes to:
- intestinal inflammation [48]
- a higher stress response
- anxiety
- a higher risk for depression (dependent on low BDNF)
- higher adiponectin
- lower BMI
- lower BDNF
- decreased hunger/increased anorexia risk
- more severe IBD [11]
- probably more fatigue (independent of lectin consumption)
As you can see, this gene causes all of the symptoms that are associated with lectin sensitivity and even some of the symptom markers such as adiponectin.
We still don’t understand how this particular variant changes the function of the CB1 gene (whether it increases or decreases function), although it is strongly associated with other health conditions listed above. Problems with CB1 activation (too high or too low) can cause intestinal permeability. In mice, activation of CB1 receptors in the gut causes intestinal permeability [49] and blocking the CB1 receptor decreased permeability [50]. This depends on how the CB1 receptor was activated [15].
The T allele causes you to not build a tolerance to pot as much (lack of receptor desensitization) and have fewer receptors (makes it less likely to activate).
Other CNR1 SNPs:
- RS12720071 (CNR1)
- RS6454674 (CNR1)
- RS806368 (CNR1)
- RS806377 (CNR1)
- RS806378 (CNR1) is associated with higher risks of IBS due to abnormal gut movement [51].
- RS806380 (CNR1)
The CB2 Receptor
Originally it was thought that only the CB1 receptor was found in the brain. Recently, the CB2 receptor has shown that it is found in neurons as well. Scientists still debate whether these receptors are found in the brain.
After taking Beta-Caryophyllene, I believe it is found in the brain.
CB2 receptors are found throughout tissues of the immune system, including the spleen, tonsils, and thymus gland, where they are primarily responsible for inhibiting cytokine release. CB2 receptors are found on immune cells such as monocytes, macrophages, B-cells, and T-cells.
In the brain, CB2 receptors are found primarily on microglia, which are the immune cells of the brain, as well as the hypothalamus [52], striatum [53], amygdala [54], prefrontal cortex [54], brainstem, VTA, basal ganglia [55], and hippocampus [54] to a lesser extent.
CB2 receptors are also found throughout the gut, where they inhibit the intestinal inflammatory response.
The CB2 receptor is a potential therapy for inflammatory bowel diseases, such as Crohn’s disease and ulcerative colitis [56, 57].
The CB2 receptor is found on mast cells and can inhibit mast cell release [58, 59].
CB2 receptor activators cause a reduction in cAMP, which results in a reduction in the binding of transcription factor CREB (cAMP response element-binding protein) to DNA. This reduction causes changes in gene expression and ultimately suppression of immune function (inhibition of T cell activation) [60].
In patient’s with Alzheimer’s disease, beta-amyloid proteins form aggregates known as senile plaques, which disrupt neural functioning. CB2 receptor activation was shown to induce macrophages to remove beta-amyloid protein from human tissues, which can help this condition.
Changes in endocannabinoid levels and/or CB2 receptor expressions have been reported in almost all diseases affecting humans, ranging from cardiovascular, gastrointestinal, liver, kidney, neurodegenerative, psychiatric, bone, skin, autoimmune, lung disorders to pain and cancer. The prevalence of this trend suggests that modifying CB2 receptor activity by either CB2 receptor activators or blockers might help these conditions [9].
The CB2 receptor help reduce addiction from cocaine.
Summary Table
| Disease | CB1R/CB2R Regulation | Proposed Role of CB1R/ CB2R in Disease | Therapeutic Implications |
|---|---|---|---|
| Neuropathic pain | CB1R and CB2R are increased neuropathic pain [61, 62, 63, 64, 65]. | Inhibition of neurotransmitter release decreases hyperexcitability of sensory pathways (CB1R); inhibition of inflammation (CB2R) [66]. | Increased CB1R enhances pain-relieving response to cannabis [62]. |
| Neuroinflammation and brain injury | CB2R increased in microglia/macrophage-like cells of patients with MS or ALS [67]. | CB2R expressed on T cells reduces inflammation in MS [68]. | Increased CB2R increases the efficacy of CB2R activator [68]. |
| CB1R increased in rat brain after mild concussive head injury and NMDAR blockade [69]. | Neuroprotection by decreasing glutamate release/excitotoxicity [70]. | ||
| Cancer | Increased CB1R and CB2R in multiple human cancers [71]. | Cannabinoid receptor activation leads to cancer cell destruction [71]. | Increased receptors may be crucial for the antitumor effects of cannabinoids. For example, cannabis inhibits the growth of prostate cancer cells with high expression of CB1R and CB2R [72], whereas THC stimulates growth in breast cancer cells with low receptor count [73, 74]. |
| Decreased CB1R in human colorectal tumors [74]. | Leads to enhanced colorectal tumor proliferation in a mouse model of colorectal cancer [74]. | ||
| Gastrointestinal | CB1R increased in a mouse model of diarrhea [75]; CB1R and CB2R increased in multiple models of colitis [76, 77]. | CB1R decreases intestinal motility, secretion, and visceral pain and promotes wound healing. CB2R expressed on gut immune cells decreases inflammation [78]. | Increased CB1R can increase the potency of agonists in slowing intestinal transit in a mouse model of diarrhea [75]. |
| Liver | Liver CB1R and CB2R increased in cirrhosis in humans [79, 80, 81]. | CB1R promotes fibrogenesis [80]. CB2R activation is anti-fibrogenic [79]. | Blocking CB1R and activating CB2R reduces fibrosis [79, 80]. |
| Liver CB1R increased in mice fed high-fat and high alcohol diets [82, 83, 84, 81]. | Blocking CB1R decreases liver fatty acid synthesis in mice fed a high-fat diet [82]. | ||
| Metabolic | Fat tissue CB1R increased in obesity [85] | CB1R increases fat cells and may increase insulin release from the pancreas [86]. | CB1R blocker for reducing weight in obese [87]. |
| Muscle CB1R increased in high-fat diet [88]. | CB1R up-regulation in muscle may contribute to insulin resistance in obesity [89]. | ||
| Cardiovascular | CB1R up-regulated in myocardium and aorta in rat model of hypertension [90]. | CB1R lowers blood pressure by decreasing cardiac contractility and vascular resistance, but this effect is only seen in hypertensive, not normotensive animals [90]. | CB1R up-regulation in the heart and vasculature may account for increased potency and efficacy of agonists in hypertensive animals [90]. |
| CB2R increased in immune cells in atherosclerotic plaques in humans and mouse model [91]. | CB2R decreases plaque progression, possibly by reducing infiltration of immune cells and cytokine release [91]. | ||
| Psychiatric | CB1R increased in the prefrontal cortex of depressed suicide victims [92] and patients with schizophrenia [93]. | CB1R has both excitatory and inhibitory effects on synaptic transmission in the prefrontal cortex [94, 95]; the effect of its up-regulation in these diseases is not known. | Targeting the endocannabinoid system in these diseases will require a better understanding of its role. |
Read 49 ways to increase or decrease cannabinoid function without pot
Relevant Resources
If you have some bad SNPs inside the cannabinoid receptor genes, especially rs1049353, and also struggle with inflammation, then I highly recommend you try the Lectin Avoidance Diet to see if some foods may be causing inflammation.
