I’ve been trying to fix my food sensitivities since adolescence, but I didn’t quite understand how. Over the past 5 years, there’s been new research come out that sheds light on how to do this.
I’ve been experimenting with this approach to good success so far. I’ve been able to tolerate a whole variety of foods that I couldn’t tolerate before.
Early on, I was sensitive to everything, except beef and chicken. Even vegetables would cause a mild reaction.
Hence, for some time I was doing a diet that was similar to a “Carnivore” diet (I called it a “Lectin Avoidance Diet”) that was practiced and made more famous by Jordan Peterson and his daughter. Peterson even got Joe Rogan to do the diet for a month and Rogan felt quite amazing for it, but stopped it because it was too restrictive.
I’ve seen the diet successfully reverse many people’s autoimmune issues, as it successfully did with mine. I know personally 3 people with multiple sclerosis that halted their disease as a result of such a diet.
When people go on a limited diet that is very low on food allergens and plant lectins, many people experience significant health improvements.
You’ll notice that many of the preachers in this space had some kind of autoimmune type issues that they solved with the diet.
A whole variety of natural foods – specifically grains, beans & nightshades – can cause inflammation for quite a lot of people. Other common allergies include eggs & dairy. Many people are sensitive to specific fruits or nuts.
There seems to be a wide range of foods that people are sensitive to and people don’t even know what. The current tests for food sensitivities are all pretty much bogus – based on my readings and conversations on the podcast.
The closest thing I’ve found to actually be good is genetic predispositions for sensitivities or allergies, but that’s still not 100% certain, because genetics can only tell you about tendencies.
So people still have to do strict elimination diets, and very few people can successfully do those.
But even if they are successful at it, restrictive diets are problematic for other reasons:
- They are actually not healthy from a general health perspective – including deficiencies
- It is socially disruptive since food is such an integral part of how people socialize
- It reduces life enjoyment
Therefore, it’s been my lifelong goal to crack the code on food sensitivities and allergies.
Over the years, I found various things that have helped, and that has allowed me to incorporate more foods in my diet. I started with vegetables, and then made my way to fruits.
But I still wasn’t eating root vegetables, nuts, seeds, eggs or dairy, and certainly not grains or beans.
Why Do Food Sensitivities Occur?
One thing I learned in my research is that food allergies, food sensitivities, and autoimmune disease have similar mechanisms by which they come about. This is not something that was clear to me in the beginning.
This is especially true for people with IBD, IBS, and other types of gut inflammation. There’s usually some food component involved.
There are clearly differences between some of these – for example, allergies are more Th2 related or Th1 for food sensitivities.
Some autoimmune conditions are Th2 dominant whereas others are Th1 or Th17. Some may have to do with various other systems.
But the underlying connector between them all have something to do with T Regulatory Cells.
This is the main mechanism by which a body can program itself to say a specific organ or food is friendly, don’t attack it!
If someone’s immune system misfires against their own body, it also likely misfires against various foods as well.
This is something that I was aware of since 2014 already, but the immune system is quite complex, and scientists are still trying to figure out all of the nuances.
Everyone has a weak point where the inflammation is directed to in the body. Sometimes it’s the gut, thyroid, brain, etc… And based on where that weak point is, the disease name is different.
But the underlying immune mechanisms are often not too different for each autoimmune disease. Often, people with one autoimmune type issue will experience inflammation in multiple places, or system inflammation.
There are many herbs that increase T Regulatory Cells, and those all helped me to some degree, but there was still something missing.
Just saying food sensitivities are from problems with T Regulatory cells (Tregs) is an oversimplification, and I’ve identified other pathways that are involved, but they all generally tend to involve increasing T Regulatory cells and their suppressive power on inflammation.
My First Breakthrough: Fish Oil
When looking at the research, the things that are most commonly known to increase Tregs and create tolerance are fish oil (mainly DHA), Vitamin D, and Vitamin A.
However, only high dose fish oil was able to lower food sensitivities for me out of the three, mainly because I already had adequate levels of Vitamin D or A.
Most people actually have enough vitamin A, but are short on fish oil (EPA/DHA) and vitamin D.
Longvida curcumin was also quite helpful in increasing tolerance to foods based on a variety of mechanisms, but it’s been researched to increase Tregs quite powerfully.
High dose fish oil and curcumin were working to some degree, but I actually started getting bruising from taking too much fish oil because my blood wasn’t clotting enough.
I continued taking 2g of fish oil and longvida curcumin since then, but it wasn’t close to being enough.
I was also taking other immunosuppressive herbs that lowered the Th1/Th17 immune system.
Second Breakthrough: Butyrate
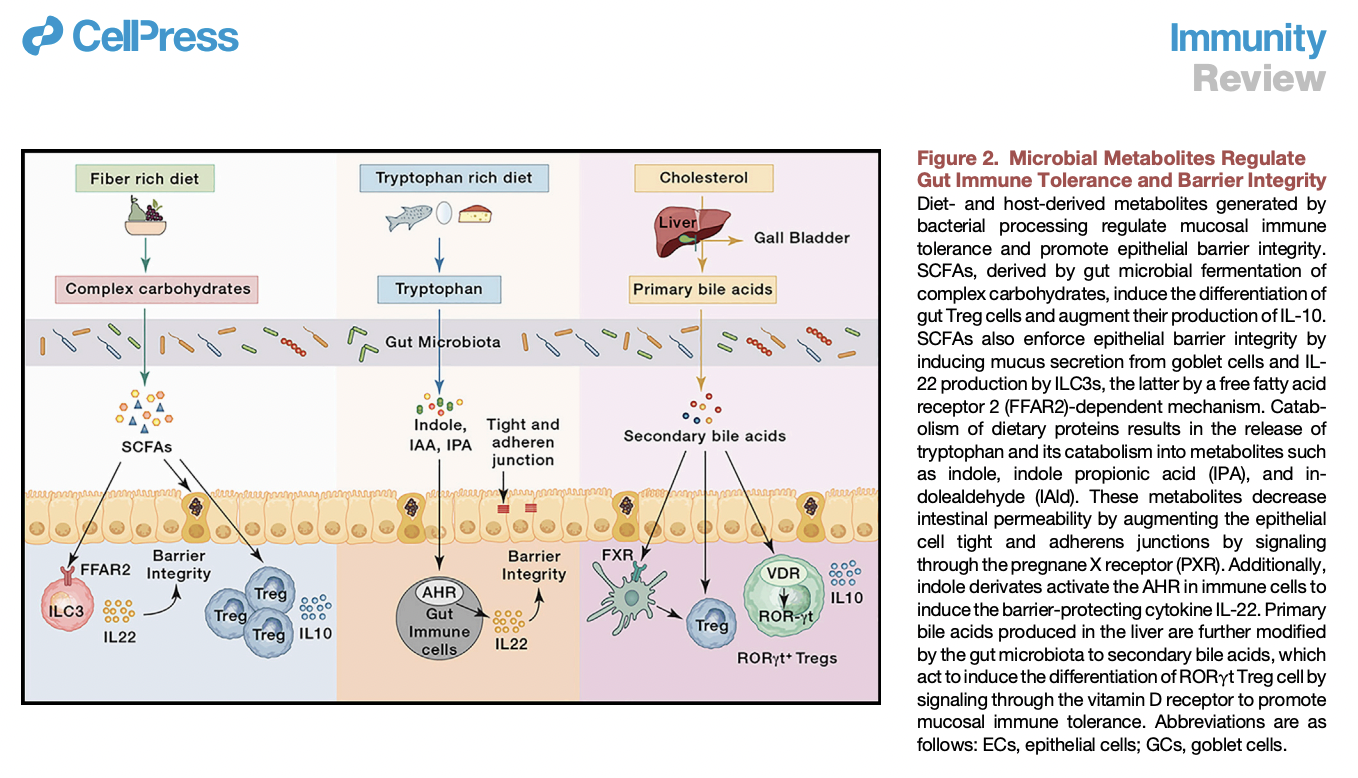
The second real breakthrough came when I started consuming Resistant Starch, which converts to butyrate. This was the one thing that really made a noticeable difference in reducing food sensitivities, more so than fish oil, curcumin, and various herbs.
For a while, I was taking 100g a day of Jo’s Resistant Starch, but it was too strong in certain ways, even though it did a great job.
Jo’s Resistant Starch was a real game changer – the best thing for food sensitivities I’ve discovered to date, but taking 100g a day wasn’t sustainable since I would get bloating and gas from that much (as a result of the butyrate production).
I then settled on 40g/day as an optimal level where there were minimal GI effects, but significant effects against food sensitivities. I was also taking a lot of butyrate capsules.
Since discovering other mechanisms, I’ve reduced Jo’s Resistant Starch to 25g/day. To this day, it is still the number one tool I use against food sensitivities.
Butyrate counteracts food sensitivities through multiple mechanisms that I won’t discuss in detail now:
However, there still seemed to be some pieces of the puzzle missing.
My Third Breakthrough: Niacin
I’ve been on a health journey for the past 9 months to take my health to the next level, using all the tools at SelfDecode to improve my health. With the help of SelfDecode, I’ve learned some more breakthroughs on how to fix food sensitivities.
One thing I figured out was that I was deficient in niacin. After trying it out, it felt like the lights went on and it worked on many areas that I was trying to improve upon.
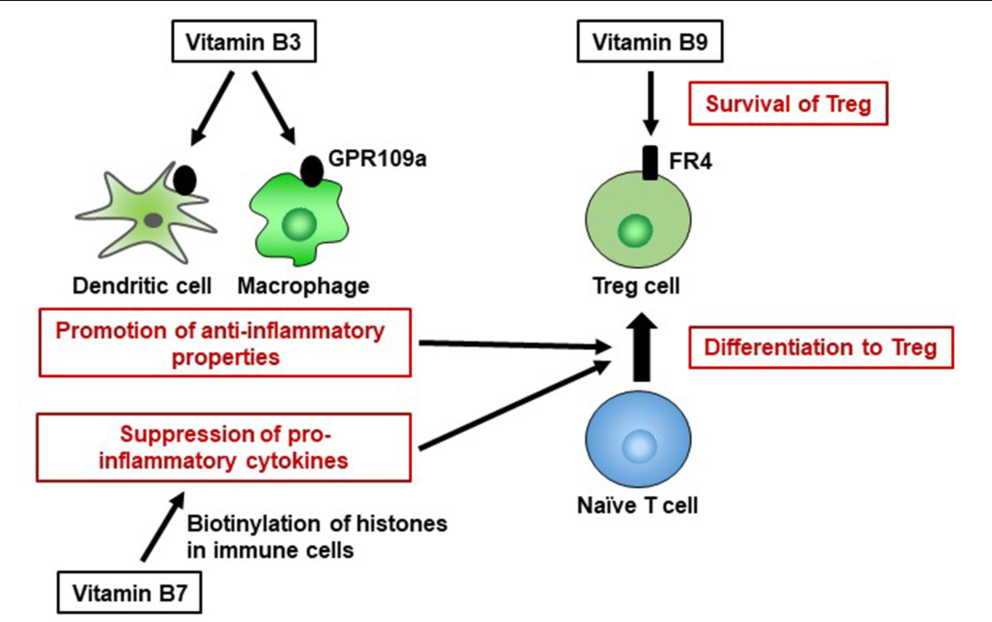
Niacin activates a specific receptor in the gut called the GPR109a or HCA2 receptor. This receptor is responsible for the flushing effect of niacin, but it also lowers inflammation in the gut and helps create tolerance via increasing Tregs [1].
Guess what also activates this receptor? Butyrate. To date, those are the only 2 activators of this receptor – and those are 2 things that are most significant for reducing my food sensitivities.
It turns out, that I’ve been chronically deficient in niacin my whole life. In addition, I figured out that I was suboptimal in methylfolate and biotin (B7), which also help increase Tregs.
My Fourth Breakthrough: Tryptophan & Probiotics
In my quest to lower my LDL cholesterol and optimize various labs, I’ve been taking huge amounts of fiber and probiotics.
I’ve been trying to get my APOB down to less than 70, and my LDL-C down to under 100.
It’s been quite stubborn to get down, and so far my lowest LDL-C has been 115.
Fiber is a fantastic way to get it down, but I started to get gas as I was consuming huge amounts of veggies and supplemental fibers.
Fibers can often slow down gut movement or motility by activating GLP-1. It felt like my GI system was being slowed down by these fibers.
If I don’t stress test my gut, it’s usually fine, but in my quest to optimize my labs, I was stress testing it quite significantly.
So I started looking at what can increase motility and improve my gut health, while still consuming large amounts of fiber.
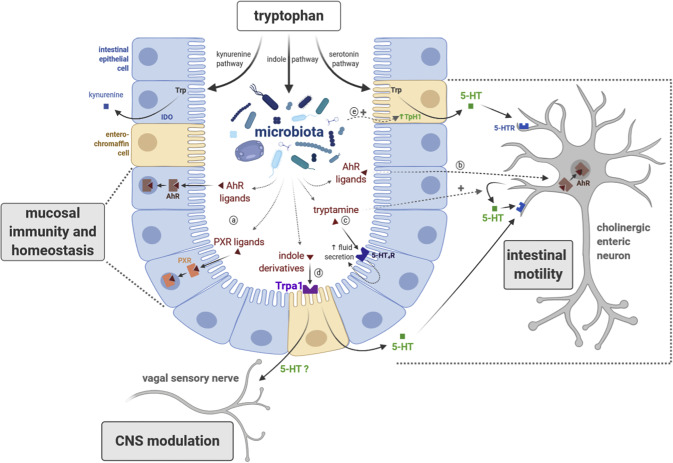
I stumbled upon tryptophan and a study called “Tryptophan metabolites get the gut moving“.
Tryptophan has been on my radar for many years for many reasons. For one, it increases serotonin, which I always knew I needed more of. Second, I recalled reading an interesting article by a professor about high APOB being a signal of tryptophan deficiency [2].
I also knew that since I was deficient in niacin, I was also likely deficient in tryptophan, because your body uses tryptophan to create niacin when you’re deficient in niacin.
By increasing serotonin, it helps with mood and sleep. However, when I tried it for sleep, it actually kept me awake and caused some kidney sensations, and I felt 5HTP was actually better at improving mood for me, so I didn’t see a need to take it.
However, tryptophan does have a dark side – it increases certain kidney toxins in the body called indoxyl sulfate. Without a very good reason to take it, I decided to let it sit in my cabinet.
After seeing how important tryptophan was in gut health and Tregs, I decided to give it another go, this time to see if it improved my gut health in response to the huge amounts of fibers I was consuming [3]. In addition, I wanted to see if it would help with food sensitivities.
Tryptophan gets broken down and gets converted to kynurenine, indoles, and serotonin. Indoles and serotonin are critical to proper gut function, and creating tolerance to foods.
While kynurenine is useful in certain ways, the indoles are much more significant for gut health. Various probiotics induce indole production instead of kynurenine production, hence why I take tryptophan with probiotics.
Indoles are one of the few things that Aryl Hydrocarbon Receptors (AhR), which are responsible for creating tolerance to foods, but also detoxing from environmental toxins.
Based on my experience, people tend to start coming down with food sensitivities after a stressful time. Why is that? Well, there are many reasons, but I think the primary one is because stress and cortisol shift tryptophan production to kynurenine and away from other things like indole creation.
When you like indoles, your gut starts to get intolerant to food.
Right after I took tryptophan, it was clear to me that I was onto something. My gut noticed relief pretty quickly and I was reacting significantly less to foods. It seemed to be that a chronic deficiency of tryptophan and niacin together created all of my food sensitivities to begin with.
Fifth Breakthrough: TUDCA
I also started reading about bile acids in many papers that were talking about tolerance in the gut. However, every time I tried to take bile acids to optimize some of my markers, it seemed to give me GI issues.
My suspicion was that the slower motility, food sensitivities, high cholesterol, somewhat lower T3, and somewhat higher pancreatic enzymes were a result of not enough bile.
When I was eating a lower fat diet, my cholesterol was at a reasonable level. But higher levels of fat spiked my cholesterol since it wasn’t being used to create bile.
So I decided to try TUDCA instead, which is one very specific bile acid that stimulates the creation and flow of bile and can actually improve all of the areas that I wanted to optimize – gut flow, high cholesterol, higher (but normal) pancreatic enzymes and lower (but normal) T3.
TUDCA didn’t have any negative gut effects and seemed to actually help gut function quite instantly.
In the study “Dietary and Microbial Determinants of Food Allergy“, you can see this put together nicely. Fiber (most importantly butyrate) + tryptophan (needs the right probiotics) + bile acids create the proper environment for tolerance to foods.
My Results So Far
Since starting this new protocol, I’ve been able to tolerate all kinds of fruits, vegetables, nuts, seeds, eggs, and even dairy. I’ve eaten specific types of beans with no significant reaction as well.
It will take a while to see the full effects of how much this protocol works, since for each food, it’s best to start slowly and gradually increase the amount over time.
I recommend starting with small quantities, the smaller the better, to give your system a chance to adjust. If you’re reacting, then start with less. The idea is that your gut needs to take the food and learn how to create tolerance to the proteins.
This approach has already helped me out quite a lot, and I’m much more resilient to all kinds of life stressors.
I also recover much more quickly and the reactions are less intense if there is a reaction.
I still will try to stay away from grains and beans, and reduce my dairy consumption, but at the very least it has already allowed me to consume a wider variety of foods without a significant negative impact.
I’m sure there’s much more to learn, but the breakthroughs have been quite significant for me so far and I felt compelled to write about them!