Are you experiencing forgetfulness, confusion or inability to focus? This is brain fog. Learn the causes & conditions associated with brain fog.
After helping 1000+ clients with brain fog, and healing my own brain fog, I’ve figured out all of the causes and the most effective solutions. In this post, I will summarize what the common causes are and the most effective solutions. To find out which brain fog causes are most applicable to you, fill out the quiz at the end of this post.
What is Brain Fog? – An Executive Summary
Brain fog covers a constellation of symptoms such as forgetfulness, a lack of mental clarity, confusion, and an inability to focus. It is also known as ‘mental fog,’ ‘clouding of consciousness,’ and ‘cognitive dysfunction.’
This post explains the causes of brain fog and provides methods for treating it.
Brain fog/cognitive dysfunction comes from inflammation and too many free radicals (oxidative stress) [1, 2].
The hypothalamus is what senses the oxidative stress and we experience brain fog.
Any time you have elevated oxidative stress, your brain fog worsens. Such instances occur during sleep deprivation, jet lag/circadian disruption, or after any event that causes inflammation.
The more complex question is why you have elevated inflammation and oxidative stress. I’ve spent years studying this, and in the past few years I’ve helped a wide range of people deal with their brain fog issues, so I’ve gained quite a bit of experience in understanding the wide variety of causes.
The most common causes of chronic inflammation and oxidative stress are as follows:
- Lectins
- Chronic infections
- Biotoxins
- Sleep problems is a significant one
- Injuries
- Low hormones
- Obesity/terrible diet
- ‘Gene-environment interactions’ or other causes (read the rest of the article)
Often, there is a mix of these.
In most cases, people with brain fog have lectin sensitivity and should try a lectin avoidance diet, or even better, an elemental diet. You don’t have to keep to these permanently, but they help you figure out if lectins are the source of your issues. Dr. Gundry is the leading expert on lectins, and you can listen to my interview with him.
Lectin sensitivity is very likely to blame if you experience fatigue after meals, stomach problems (gas, bloating, etc.), anxiety, and inability to let go of thoughts.
People with lectin sensitivities develop immune imbalances. Some people are Th1 dominant, while others are Th2 dominant. Read this post to find out which immune profile you have.
People obviously have a genetic predisposition for one immune profile or another, but dietary lectins usually exacerbate it. Milk and various other dairy products almost always make the problem worse.
If you don’t have lectin sensitivity or an immune imbalance, then the second and third most common explanation is an infection of some kind or sleep problems.
Whether you have lectin sensitivity or not, a Ketogenic Diet is almost always helpful. I’ve had a hard time with this in the past, so I’ve developed a protocol to get into it more easily. However, most will find a ketogenic diet too difficult in the long term.
Otherwise, various lifestyle and environmental factors may increase inflammation and oxidative stress. These factors are sometimes the starting point of people’s health issue, but mostly they are just contributing factors.
You can check for lectin sensitivity by testing your genetics: CNR1 gene (RS1049353 in particular).
After dealing with a lot of people I realized everyone has somewhat different issues and symptoms. Often issues are multi-factorial. The first issue will trigger a cascade of events and people are left dealing with downstream events that are causing chronic issues.
Brain Fog Test: Do You Have Brain Fog? And Are the Remedies Helping?
I find that most of my brain fog clients have trouble telling if something is somewhat helpful with their brain fog. They would be able to tell if a supplement or device completely takes away the brain fog, but not if it partially improves their brain function. Brain fog is a complex problem and most people will need multiple interventions to completely fix it. Therefore, I recommend using Brain Gauge to quantify if any supplements, devices, or lifestyle changes help with your brain function to any degree, so that you can create your own brain fog protocol that works. You can read about Brain Gauge here and purchase it here. Use code SELFHACKED to save 10% off any Brain Gauge device.
The Cause of Brain Fog
In a sentence, brain fog is a condition caused by oxidative stress and inflammation. Oxidative stress is when you have too many free radicals and not enough antioxidants.
Free radicals are highly reactive molecules (due to an exposed electron) that disrupt the normal process within a cell. Antioxidants are molecules that interact with a free radical and stabilize it so it can’t cause any harm.
The body has a ‘sensor’ that senses inflammation and oxidative stress in order to respond accordingly.
The hypothalamus is that sensor. It’s located in the core of your brain. If the hypothalamus senses inflammation it will respond by shutting our system down (by suppressing orexin).
Inflammation is usually the starting point, which leads to oxidative stress. Oxidative stress (OS) in the hypothalamus is what we experience as brain fog.
Both OS and inflammation can breakdown the mitochondria. The mitochondria are “the power plants” of the cell and provide energy for the brain and other organs. When your mitochondria break down, it causes even more OS and inflammation, leading to a vicious cycle [3].
You will, therefore, feel cognitive fatigue as well as brain fog.
Bottom Line: whatever exacerbates oxidative stress or inflammation makes brain fog worse.
Read this post for more in-depth information on the causes of brain fog.
Superoxide: The Worst Free Radical
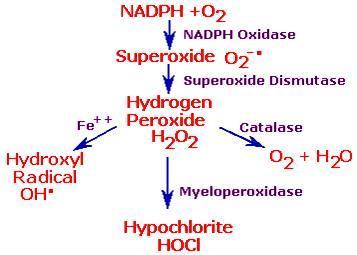
There are many types of free radicals, but the most significant free radical is ‘superoxide’ (or O−2).
Superoxide has some useful roles in the body. For example, superoxide is used to damage foreign invaders such as bacteria, which is why your body produces it when you’re sick. Anytime we eat or breathe, we create superoxide because it’s a byproduct of the energy production process (metabolism).
However, brain fog occurs when too much of it is chronically produced and not enough is neutralized. Just like superoxide is damaging to bacteria, it’s also damaging to us, and the damage accumulates. The accumulated damage is the most significant reason people age.
Superoxide is very damaging to our proteins and mitochondria. Superoxide is also the starting point for all of the other main free radicals/reactive oxygen species (ROS) that damage us.
Superoxide degrades collagen and hyaluronic acid, causes cytokine release/inflammation, fat peroxidation, and DNA damage.
Superoxide is damaging enough on its own, but it also goes on to produce other harmful free radicals/ROS including peroxynitrite (ONOO¯) and hydrogen peroxide (H2O2), which in turn creates hydroxide radicals (·OH).
Superoxide converts to peroxynitrite. Peroxynitrite(ONOO¯) decreases MnSOD (antioxidant defense), decreases the cortisol receptor (causes glucocorticoid resistance), and increases COX2 and prostaglandin production. It also decreases glutamate transporters and glutamine synthase (both of which increase glutamate outside the cell=bad), decreases tyrosine hydroxylase and norepinephrine formation.
Superoxide converts to Hydroxyl Radicals. Hydroxyl Radicals (·OH) cause protein damage, cell membrane damage, DNA damage, and mitochondrial damage.
What’s the Source of the Inflammation and Oxidative Stress?
Chronic inflammation (and oxidative stress) most commonly comes from:
- Lectins
- Chronic infections
- Biotoxins
- Sleep problems
- Injuries
- Low hormones
- Obesity/terrible diet
- ‘Gene-environment interactions’ or other causes
Almost always, there is a mix of these factors.
In maybe 65 percent of the cases I had, brain fog was caused in large part by lectin consumption, but usually, that’s not the full story.
The Most Common Causes of Brain Fog
There are many other possible sources for brain fog. However, I’ve only listed the most common ones that wouldn’t be diagnosed by your doctor.
Brain Fog and Food
The most common cause of brain fog is lectin sensitivity.
Sometimes, people only have to stay away from specific proteins or antigens and they’re fine. Some common ones are:
- Gluten (wheat, spelt, rye, barley, and oats)
- Casein (all dairy products)
- Yeast (in gluten-free breads)
- Lectins (every food has lectins, but we can be sensitive to different lectins.)
- Food additives like carrageenan (in rice milk, almond milk, etc..)
- Salicylates
- Caffeine
You can be allergic to any other foods as well. Egg and fish allergies are quite common, so pay attention to them.
You should try out a lectin avoidance diet or better yet, an elemental diet.
These diets are highly restrictive, but in the long term, you eat whatever you want. I just think it’s a good idea to keep these diets until you can tell if lectins are the cause of your issues.
Follow an elemental diet for two weeks, and then add one food at a time back in to see if your issues are from food allergies, lectin sensitivity, or something else.
In some cases, brain fog simply comes from a horrible diet. High glucose levels cause a threefold increase in ROS levels, which may damage human cells [4].
If you’re living on a Standard American Diet, then that’ll likely be a significant contributing factor to your brain fog.
Also, if you can do it, caloric restriction is a good method to decrease oxidative stress and inflammation in the body [5, 6, 7].
Lectin-Induced Brain Fog
Lectins are plant proteins that induce an immune response. Most of the time, the immune response is not systemic – or if it is, it’s not too bad.
Instead, plant lectins resemble certain tissues such as the synovium in joints and the thyroid.
People with lectin sensitivity most often experience inflammation in their stomach joints, thyroid, and hypothalamus. Sometimes they go on to develop an autoimmune condition of one sort or another.
Lectin sensitivity starts out without many direct markers and modern medicine does not yet know of all the types of antibodies produced against different tissues.
People with one autoimmune condition are at increased risk for another. So if you have Hashimoto’s disease in your family, you are more likely to have a hypothalamic problem.
Sometimes, however, the autoimmune issue is strictly in one tissue over another.
See if you have the markers for lectin sensitivity, and listen to my interview with Dr. Gundry.
Brain Fog and Genetics: MTHFR, SOD2, APOE4, and Other Mutations
There are many genes that don’t interact with our current environment well; i.e., they are outdated.
Two significant ones are MTHFR and SOD2 mutations. There are many others, but that’s beyond the scope of this post.
Genetic mutations interact with the environment in very significant ways. Knowing you have a mutation helps guide you on a more focused course of action for your brain fog.
Having the MTHFR mutation seriously hampered my ability to ‘detox’ and results in inflammation and oxidative stress.
The SOD2 mutation causes a 33 percent decrease of the enzyme (MnSOD) that breaks down superoxide in the mitochondria. Superoxide production is the most significant cause of brain fog.
In 2014, two studies found that the level of genes production of SOD2 (MnSOD) is strongly correlated with cognitive performance [8, 9].
The main SOD2 variant rs4880 GG is more common in my brain fog clientele and there’s a lot of scientific research on it.
Three other SOD2 variations are also heavily over-represented in my clientele and include rs2758331 (AA), rs2758339 (CC), rs10370 (AA). However, some science has been performed on these, and the most important variant is rs4880 (CC).
A study in 2014 found that the production of another anti-oxidative enzyme gene that breaks down H2O2 (MPO/Myeloperoxidase) was also strongly tied to cognitive performance. Having a mutation in these genes could result in cognitive impairment [10].
And yet another 2014 study found that mutations in genes that code for melatonin (ASMT)–an internal antioxidant hormone–were tied to cognitive impairment [11].
Obviously, your genes are only a part of the story. It’s usually the case that you need to have these mutations and other factors that increase oxidative stress.
PON1 mutations, while not as significant as SOD2 mutations, impair our ability to break down pesticides. This suggests that people with this should only eat organic food.
Through my genetic data, I was able to see that I had various mutations (such as MTHFR, SOD2, and PON1).
I discovered that I had many genes for Th1 dominance in my genetic data and none for Th2 dominance. I discovered that I had many mutations that can cause gut inflammation.
I found mutations in my ability to ‘detox’ and in antioxidant genes. This tells me that the genetic data is accurate because I already knew I was Th1 dominant, I had elevated levels of oxidative stress and was sensitive to many chemicals.
In addition to these, I found many other genes that showed I was Th1 dominant, which I already knew, but my DNA confirmed this. I also had many genes involved in inflammation of the stomach, which I also already knew. However, it taught me a few things I didn’t know, such as what the underlying driving force was for my Th1 dominance is (STAT4, IL-23, IFNa, etc.). This information allows me to make a more targeted protocol.
Is your brain fog from lectins, an infection, or something else? The genetic data helps you figure that out. It’s a significant piece of the puzzle.
The good news is that genes can be overcome with lifestyle and supplement choices.
Brain Fog and Sleep
Not sleeping well is one of the most common causes of brain fog.
If you have sleep apnea, then that is often the cause of your brain fog. Sleep apnea causes hypoxia or a lack of oxygen at night, which increases ROS/oxidative stress [12].
Hypoxia drives psychiatric conditions by causing neurons to get overexcited (glutamate excitotoxicity).
Even if you don’t have sleep apnea, bad sleep is still a significant cause of brain fog, but may not be the whole story.
Sleep loss increases oxidative stress in the hypothalamus, by the loss of glutathione [13].
Sleep deprivation for even one night exacerbates brain fog by increasing inflammation in the hypothalamus as well as inflammation in the whole body [14, 15].
People with morning brain fog should particularly watch out for this.
Adequate sleep in my book means getting the amount of sleep you’d get if you didn’t have an alarm clock.
I suggest doing a sleep study and checking how much slow wave and REM sleep you’re actually getting, and also rule out any potential sleep disorders.
Brain Fog and Infections
Science is increasingly becoming aware of the link between various autoimmune conditions and infections – usually earlier in life.
When someone was healthy their whole life and suddenly comes down with brain fog after an infection, effort should be made to identify and get rid of the infection. In the case of viral infections, you should control it.
Infections may cause chronic inflammation and oxidative stress, leading to brain fog.
Viruses
Sometimes, infections such as viruses are latent and then reactivated by some stressor (lack of sleep, poor diet).
Viruses can modify the immune system to become more sensitive or malfunction, which causes downstream problems.
People with Th2 dominance often can’t control viral infections well and experience chronic inflammation. This is likely the case with chronic fatigue syndrome.
Epstein-Barr Virus is a common viral infection that causes harm. Even if it’s another virus, controlling viral infections have common themes.
People with severe immunodeficiency struggle with controlling viral infections.
Since you can’t rid yourself of a virus, you want to instead make sure your immune system always keeps it at bay.
Testing your Natural Killer Cells and their activity are some important indicators into how you handle infections — both viral and other.
If this is the cause of your issues, then you want to rebalance your immune system.
Bacteria
I’ve seen many cases where brain fog was caused by a bacterial infection.
If you can identify that you have a bacterial infection, then targeted drugs such as antibiotics are a better option than herbs.
Gram-negative bacteria are also known to cause overproduction of TNF, IL-1, and IL-6 [16].
Only gram-negative bacteria have lipopolysaccharides, which is a significant reason why they cause inflammation.
Some common infections include Lyme, Mycoplasma pneumoniae, and H Pylori.
Fungal
I’ve seen other cases where candida or fungal infections were the sources of the brain fog.
Candida comes from an immune deficiency. Environmental triggers include refined carbs, stress, low stomach acidity, which could be from antacids, and antibiotics.
Anybody with brain fog after antibiotic treatment and/or a particularly stressful period should look into candida as being the cause.
People with candida or bacterial infections often have a chronic type of brain fog. Candida increases TNF, IL-1, and IL-6 [17].
Candida and bacterial infections are usually cured through conventional and alternative means. The latent viral infections are the tricky ones.
Parasites and Protozoa
Although less common in the developed world, parasitic infections can also be problematic.
Other times, parasites or protozoa are a problem. These include Blastocystis hominis, Tapeworm, Roundworm Antibodies, Tissue worm, and Toxoplasma.
Brain Fog and Biotoxins: The Role of Mold
People exposed to mold or other biotoxins and who go on to develop Chronic Inflammatory Response Syndrome (CIRS) develop a certain kind of brain fog.
In people who get brain fog from mold, they have many specific characteristics such as rapid weight gain, muscle loss, and Th2 dominance.
CIRS is characterized by high C4a, ACTH/Cortisol, TGF-beta, MMP-9, VEGF, and low MSH, ADH (aka vasopressin), and VIP.
I discuss mold-induced illness in a different post and what to do about it.
All kinds of toxins have the ability to stimulate the immune system and cause oxidative stress.
Brain Fog and Low Acetylcholine
People with chronic inflammation and brain fog (often from chronic infections) sometimes exhibit a mix of symptoms that almost exactly match symptoms from drugs that inhibit acetylcholine.
People with biotoxin issues usually fit into this category, but most people with brain fog do not experience all of these symptoms because of different issues.
Acetylcholine inhibits inflammation/cytokines and controls the immune response [18].
Cytokines also decrease acetylcholine.
TGF-b inhibits acetylcholine formation, at least in muscle and spinal cells [19].
IL-1 induces the enzyme that breaks down acetylcholine (acetylcholinesterase) and also increases the enzyme’s activity, thus promoting a cholinergic deficit. In addition, IL-1 directly inhibits acetylcholine release from neurons [20].
In MS, there is an inverse correlation between cytokines and acetylcholine. They have increased levels of IL-1β and IL-17 and they also have less acetylcholine in their blood and spine [18].
I recently had a client whose issues came about after botox injections. Botulinum toxin A has anticholinergic properties (inhibits acetylcholine release) [21].
Interestingly, acetylcholine is capable of inhibiting biofilm formation from candida in moths [22]. This is interesting because acetylcholine could be anti-fungal as well.
Symptoms of anticholinergic drugs are similar to symptoms experienced by bad cases of biotoxin illness:
- Poor coordination
- Dementia
- Increased body temperature (although inflammation causes lower thyroid hormones, which should diminish this symptom for some)
- Sensitivity to bright light (photophobia) from pupil dilation
- Loss of focusing ability blurred vision
- Double vision
- Increased heart rate
- A tendency to be easily startled
- Flushing
- Dry-mouth
- Diminished bowel movement (decreases motility via the vagus nerve)
- Increased intraocular pressure
- Confusion
- Disorientation
- Agitation
- Euphoria or dysphoria
- Respiratory depression
- Memory problems
- Inability to concentrate
- Wandering thoughts; inability to sustain a train of thought
- Irritability
- Mental confusion (brain fog)
- Muscle jerking/twitches
- Unusual sensitivity to sudden sounds
- Illogical thinking
- Visual disturbances
- Periodic flashes of light
- Periodic changes in the visual field
- Visual snow
- Restricted or “tunnel vision”
- Visual, auditory, or other sensory hallucinations
- Warping or waving of surfaces and edges
- Textured surfaces
- “Dancing” lines or “spiders”
- Lifelike objects indistinguishable from reality
- Hallucinated presence of people not actually there
- Orthostatic hypotension (sudden dropping of systolic blood pressure when standing up suddenly)
- Rarely: seizures, coma, and death
- Urinary retention
- Decreased mucus production in the nose and throat; consequent dry, sore throat
- Dry mouth with possible acceleration of dental caries
Brain Fog, Insulin Resistance and Low Blood Sugar
People with brain fog often get hypoglycemic because the hypothalamus is not functioning as it should. The hypothalamus is the organ that senses blood glucose levels.
When the hypothalamus is hypersensitive to glucose because of oxidative stress, it leads to hyperinsulinism and low blood sugar [23].
Insulin resistance also contributes to brain fog. Insulin resistance is when insulin doesn’t do a good job at bringing glucose into cells.
When you are insulin resistant, you experience more significant blood glucose fluctuations, which is even worse than sustained high levels of glucose [24].
These swings in blood glucose levels result in oxidative stress and inflammation and, therefore, even more brain fog [25].
Every time you experience low blood sugar, you damage your brain.
Low blood sugar drives psychiatric conditions by causing neurons to get overexcited (glutamate excitotoxicity). This excitation causes increased levels of free radicals and mitochondrial breakdown [26].
This is the most damaging aspect of low blood sugar.
The pituitary and adrenal glands are particularly involved in glucose control, but these are managed by the hypothalamus.
Realize that low blood sugar contributes to brain fog, but it almost always isn’t the original cause. Inflammation is the source, usually.
If you’re getting hypoglycemic, the most effective ways to counteract it is with exercise, kombucha (for lactate), Jo’s resistant starch, and a ketogenic diet.
Read my post on how to fix insulin resistance and what causes insulin resistance to occur in the first place.
Brain Fog and Hormonal Imbalance
A deficiency of hormones such as pregnenolone, progesterone, melatonin, oxytocin, DHEA, testosterone, estrogen, and IGF-1 may contribute to brain fog.
Melatonin, progesterone, estrogen, DHEA, Luteinizing Hormone, and oxytocin all have antioxidant effects [27].
Genes that resulted in lower melatonin, for example, were found to be associated with cognitive dysfunction [28].
More specifically, these hormones inhibit superoxide (and other free radicals): Melatonin, pregnenolone, progesterone, DHEA, testosterone, estrogen, androstenedione, DHT, IGF-1, and oxytocin [29, 30, 31, 32, 33, 34, 34, 34, 35].
All of these listed hormones are anti-inflammatory as well. Pregnenolone actually converts to all of the above hormones (except IGF-1 and oxytocin), which is part of the reason why I am such a fan.
Almost always, pregnenolone levels are also low in people with brain fog. Pregnenolone is the most important hormone.
Thyroid hormones, growth hormone, prolactin, and chronic estrogen (birth control, HRT) all actually increase superoxide [36, 37, 37, 38].
However, all of these hormones are necessary for proper brain function in normal amounts. For this reason, these hormones should be balanced rather than too low or too high.
With regard to thyroid hormones, low or high thyroid hormones may cause oxidative stress [39].
People with brain fog often have low levels of thyroid hormones. However, low thyroid hormones are a result of inflammation, not the cause of it. Actually, having a high level of thyroid hormones increases inflammation [40, 41].
Brain injuries from car accidents, being in the military, being a competitive athlete, fighting (professionally or not), or any kind of hit to the brain may lead to low hormones. If you’ve received head blows from one source or another, you must check your hormones.
I believe the most common, fundamental cause of low hormones, however, is generally chronic inflammation. Chronic inflammation (and oxidative stress) most commonly comes from injuries, sleep problems, low hormones, obesity/terrible diet, chronic infections, lectins, or other causes. Often, there is a mix of these.
Brain Fog, Leaky Gut, and Dysbiosis
With regard to stomach health, intestinal permeability or “leaky gut” and/or an imbalance of your gut microbiota (“gut symbiosis”) may increase inflammation, thereby contributing to brain fog.
Lectins are the most common reason for having a leaky gut, in my opinion.
To prevent microbial imbalance or dysbiosis, the stomach needs the right ingredients to work well (like probiotics), which is also why the right foods matter.
Probiotics are also great at helping to modify inflammation.
I’ve noticed that many/most people with brain fog also have IBS (including my former self). This is because inflammation of the gut contributes to IBS [42].
Also, hypothalamic inflammation confuses the hormones, causing changes in motility, which also leads to IBS.
For stomach health, I recommend Jo’s Resistant Starch, consuming leafy greens and taking probiotics.
Brain Fog, Allergies, and Histamine
People with asthma and allergies commonly report brain fog, which is in part from the production of histamine.
Allergies and asthma are as a result of Th2 dominance.
Histamine is produced from lectins or allergic reactions as a result of an elevated Th2 immune system.
People also consume foods with histamine, which are mainly fermented and cured foods and beverages.
If you don’t have enough of an enzyme to break histamine down, then this can be the cause of your brain fog. I’ve found this to be the case for some people.
The mechanism by which histamine causes brain fog may be as a result of oxidative stress [43].
Otherwise, when mast cells activate, they release superoxide, which supports my central theory of brain fog (that superoxide is responsible) [44].
If your histamine issues are as a result of high histamine foods, then you need to take the DAOsin enzyme. Read my post on reducing histamine. Also, read my post on reducing Th2 dominance.
Brain Fog, Anxiety, Chronic Stress, and Depression
In almost all cases of brain fog, people experience anxiety and often depression/bad moods.
This is mainly because inflammation and oxidative stress increase our stress response and cause anxiety. This also leads to depression. This certainly happened to me.
Indeed, that’s why cognitive dysfunction, depression, and anxiety often go together [45].
Inflammation (TNF, IL-1) activates the stress pathway and causes us to be more anxious and depressed. Cytokines also degrade the hippocampus and other areas of the brain, which cause depression [46].
Oxidative stress also causes anxiety [47].
Superoxide and free radicals exacerbate your biological reaction to stress [48, 49].
Chronic stress or frequent activation of the hypothalamic–pituitary–adrenal (HPA) axis causes oxidative stress as well [50].
Psychological stress increases NADPH oxidase, which results in elevated superoxide in the hypothalamus and HPA mismanagement [51].
Chronic stress elevates inflammation in the long run by causing glucocorticoid resistance [52].
Depression may be caused by inflammation and oxidative stress. However, it likely contributes to oxidative stress as well [53, 54].
Sometimes depression is the source of brain fog, but this isn’t usually the case. In most cases, it’s just a contributing factor.
Chronic stress is usually more of a problem in people who are Th2 dominant and have an immune deficiency because cortisol decreases our immune system.
Read my post on why stress is bad and my post on Corticotropin-Releasing Hormone (CRH).
Brain Fog, Heavy Metals, and Toxins
Heavy metals and toxins increase oxidative stress in the body. Since heavy metals bioaccumulate, they may cause increased levels of oxidative stress in the body.
However, while heavy metals may be a contributing factor, I’ve never had a case where it was the sole cause. Unless you have a specific reason to believe that you’ve been exposed to excess heavy metals, it’s probably best not to assume that this is the only cause.
Even necessary minerals also accumulate in the body and cause oxidative stress in the long term, but again this would just be a contributory factor.
The recommendations for this type of brain fog are in part 2.
Toxins such as Pthalates and BPA pesticides and others also cause oxidative stress. However, while these are usually contributory in a minor way, they are not the main cause.
Brain Fog and Drugs
There are many drugs that cause or contribute to brain fog.
Alcohol is a neurotoxin and increases inflammation and oxidative stress [55, 56, 57].
If you’re an alcoholic, then it will most likely be the cause of your brain fog. However, in other cases, alcohol is just a contributing factor, but far from the main cause.
Many drugs cause oxidative stress, but antibiotics are the most commonly taken ones that do.
Antibiotics, for example, produce superoxide and H2O2 and may damage your mitochondria [58].
Three different classes of antibiotics were tested: ciprofloxacin (a fluoroquinolone), ampicillin (a β-lactam), and kanamycin (an aminoglycoside). All three bactericidal antibiotics induced a dose- and time-dependent increase in free radical production.
The fluoroquinolone antibiotics and some other antibiotics may damage the mitochondria and produce free radical leakage.
I’ve also seen brain fog induced by marijuana, LSD, and ayahuasca. The mechanism is almost certainly related to hypothalamic and limbic system problems, but the exact reason why only a tiny fraction of people experience this remains a mystery.
Biological Factors That Contribute to Brain Fog
The following are biological factors that make brain fog worse and are a contributory cause of brain fog.
Brain Fog and Low NAD+ Levels
When you have low NAD+ levels, your mitochondria don’t work well and you create too much superoxide.
You’re more susceptible to infections and toxins, and you are more likely to have chronic inflammation.
Your general energy levels decline and you feel more tired.
Ubiquitination increases and you lose weight. Insulin and leptin sensitivity drop. A bunch of negative metabolic changes take place.
NAD+ levels decline with age and they are caused in part by oxidative stress over time [59].
Having high blood sugar levels results in higher NADH and lower NAD+ [60].
Insulin also increases the NADH/NAD+ ratio [61].
Having low oxygen in your cells also results in higher NADH and lower NAD+.
Blood sugar dose-dependently worsens (increases) your NADH/NAD+ ratio in the same way as low oxygen. When you combine excess carbs/sugar and low oxygen, you start getting fatigued and have low energy.
This is one of the most significant reasons why sugar/carbs makes people with brain fog feel worse.
In fact, you might feel worse after eating anything because eating decreases NAD+ levels and fasting increases it. Of course, inflammation also makes you fatigued by shutting orexin down.
Fasting, calorie restriction, and exercise help brain fog sufferers because they all raise NAD+ levels [62].
On the other hand, some people do worse in the short term because skipping meals causes low blood sugar, and when I was in a bad state, I’d feel like crap if I skipped meals. Then, I’d eat a meal and crash because there weren’t enough energy-related molecules (ATP levels) in my lateral hypothalamus from fasting, which results in the shutting down of orexin down.
Brain fog people also do very poorly with alcohol, since alcohol decreases NAD+ [63, 64].
Alcohol has a host of other negative effects, but they don’t explain the rapidity by which people feel worse from it. NAD+ explains the almost instant effects in people with brain fog.
This is also why a lot of my clients claim to do better with niacin/nicotinamide in the short term: because it increases NAD+ [65].
People often claim to do better with amphetamine usage as well. Amphetamines use up energy, ATP and also deplete dopamine in certain parts of the brain (striatum in rats) [66].
When rats were given niacinamide to increase NAD+ levels, the negative changes caused by amphetamines were reduced [66].
So, we see that lower levels of NAD+ decreases brain energy and dopamine, and people start to need amphetamines to keep up.
Saunas are also considered a panacea and have been a part of every historical culture. We think it’s because we’re sweating out toxins, and that might have something to do with it, but saunas and heat shocks also increase NAD+ levels [67].
Since infrared also increases SIRT1 [68], infrared saunas are ideal.
Fermented foods and beverages such as kombucha contain NAD+, which is one reason why it energizes me. Fermentation uses NADH to produce lactate, and the byproduct is NAD+.
However, some fermented byproducts cause problems in mold/histamine intolerance and Th2 dominant people.
To increase NAD+, try Nicotinamide Riboside.
Brain Fog and Low Oxygen
People with brain fog often have hypoxia.
When you have low oxygen (hypoxia), your mitochondria don’t work as well and for good reason. Oxygen needs to be there to accept electrons in the mitochondria. When you have low oxygen, it can’t accept electrons, so your body wants to slow mitochondrial function down.
When you have low oxygen, your body responds by slowing the conversion of NADH to NAD+ (less oxidation). Therefore, you have a buildup of NADH and a relative reduction of NAD+.
We need superoxide/free radicals to defend against infections and oxygen is needed to create superoxide.
Hypoxia also causes less activation of MHC II, which lowers our ability to clear pathogens.
Read this post for reasons why you may have hypoxia and how to check for it.
Use an oxygen concentrator and breathing exercises with a breathing exerciser to increase oxygen levels.
ICES increases oxygen in cells.
Brain Fog and Low Cyclic AMP
Low cyclic AMP is a root cause of brain fog, and this is caused by poor mitochondrial function (lower ATP production).
When cyclic AMP is low, most of your hormones are lower, inflammation increases, and you can’t deal well with infections, toxins, or other cellular stressors.
Forskolin increases cyclic AMP, but you also need to make sure your mitochondria are working, or it simply uses your ATP stores up.
Conditions That Increase the Odds of Brain Fog
Some conditions like Glucose-6-phosphate dehydrogenase (G6PD) deficiency and Thalassemia increase the risk of brain fog for somewhat different reasons.
G6PD deficiency results in higher levels of oxidative stress because of less reduced glutathione.
Thalassemia results in lower red blood cells and hemoglobin, which means less transport of oxygen. This increases the risk of hypoxia in various tissues.
Anemia also increases the risk of brain fog for the same reason: increased risk of hypoxia in various tissues.
Gilbert’s Syndrome is associated with brain fog possibly because it’s often caused by low glucuronidation, high Beta-Glucuronidase, and not enough light.
Ehlers-Danlos Syndrome is associated with brain fog because of its effects on collagen formation, which affects many systems in the body.
Common Side Effects of Hypothalamic Disruption and Brain Fog
When I used to experience brain fog, I had a host of other symptoms that at the time I didn’t realize were related.
The hypothalamus plays a critical role in the following:
- Thermal control
- Sweating
- Wakefulness and fatigue
- Circadian Rhythm (manages sleep-wake cycle)
- Thirst
- Hunger and satiety
- Blood pressure and heart rate
- GI stimulation
- Emotions
- Sex drive and hormones
- Antidiuretic hormone
- Glucose management
- Vision [69]
I’ve noticed with myself and my clients that people with brain fog are more likely to have:
- Fatigue in the day: The hypothalamus controls wakefulness with orexin; inflammation (TNF) suppresses orexin neurons
- Anxiety: Inflammation can activate your stress response and lower neurotransmitters
- Low motivation: Orexin is a significant factor in motivation and it’s suppressed by inflammation
- GI problems: The hypothalamus controls vasoactive intestinal peptide (VIP) and CRH, which influence stomach function as well
- Cold hands and feet: The hypothalamus controls the body’s temperature; low orexin causes lower body temperature, and therefore you’ll feel cold [70]
- Decreased/increased appetite: Low hypothalamic serotonin leads to increased carb cravings; the hypothalamus is also the base of Orexin, T3, insulin, ghrelin, MCH, FGF21, and NPY, all of which increase appetite, while leptin, insulin, norepinephrine, serotonin, GLP-1, and FGF19 are appetite suppressants
- Decreased sex drive from low hypothalamic dopamine
- Increased thirst from low ADH, which is secreted by the hypothalamus
- Increased urination (Low ADH)
- Low blood pressure (Low ADH)
- Insomnia from stress response activation, which can come from inflammation
- Hormonal issues: The hypothalamus is the center for hormonal control; it controls male and female hormonal production, the thyroid, pituitary, and adrenal glands
- Blood sugar swings and low blood sugar: The hypothalamus controls glucose balance [71]
- Attention problems through orexin and melanin-concentrating hormone, low levels of dopamine, and acetylcholine. Orexin increases acetylcholine, and so inflammation leads to lower levels of this neurotransmitter [72, 73, 74, 75]
- Visual problems: The hypothalamus is connected to your visual system; for example, when you get tired you notice an effect on your eyes – they get heavy [69]
As you can see, the symptoms that people commonly experience with brain fog are directly tied to hypothalamic function.
I had GAD/OCD/anxiety issues, GI problems (IBS), cold hands and feet, decreased blood pressure, insomnia at night and fatigue in the day, decreased appetite (relative to others), I was thirsty all the time, and I’d pee all the time.
I couldn’t figure out why I was so thirsty. The more my brain fog improved, the more the other symptoms improved in lockstep.
I also would get hypoglycemic and feel very weak when I ate any food with a high glycemic index.
Brain Fog and Adrenal Fatigue
The hypothalamus directs the adrenal glands. Adrenal fatigue is a misconception and the root cause of fatigue has to do with the hypothalamus, not your adrenals.
Brain Fog and Derealization/Depersonalization
People who have strong levels of depersonalization and derealization have a bit of a different category of brain fog. See my post on the biology of depersonalization and its potential solutions.
Conditions Associated with Brain Fog and Caused by Oxidative Stress and Inflammation
Brain fog is much more likely to be experienced with other conditions. This is the case with conditions that are heavily associated with oxidative stress and inflammation.
There’s evidence that chronic fatigue syndrome and fibromyalgia are caused by oxidative stress and inflammation. For chronic fatigue, see [42, 76, 77, 78].
For fibromyalgia, [79, 80, 81, 82, 83].
Inflammation hits the brain stem as well in CFS [84].
It’s no wonder why brain fog is commonly cited in people with chronic fatigue syndrome and fibromyalgia – the same processes are driving all three.
Brain fog may be exacerbated by mood disorders such anxiety, OCD, depression, schizophrenia, bipolar, and alcoholism, because it is widely believed that oxidative stress plays a role in these disorders [85, 57, 86].
Actually, science is discovering now that many antidepressants work by combating oxidative stress [86].
I’ve noticed a strong correlation with these disorders – especially OCD, anxiety, and depression – and brain fog in my clients. I had all three when I used to have brain fog.
It’s not surprising that all of these conditions also have a connection with inflammation [87].
In multiple sclerosis, Sjogren’s, and lupus, brain fog is the common feature. In all of these disorders, inflammation and oxidative stress are increased.
Women with menopause sometimes develop brain fog.
Female hormones such as estrogen and estradiol tend to display antioxidant activities and lower oxidative stress [88].
When a woman goes through menopause, a reduction of these hormones shifts the balance in favor of oxidants to antioxidants [89].